Elderly patient monitored remotely
While early Hospital-at-Home programs, like the original Johns Hopkins model, operated without remote patient monitoring, today’s more advanced initiatives now commonly leverage ‘Proactive Continuous Monitoring’ (the use of real-time data from patient monitors to track vital signs and alert clinicians to potential issues), to provide comprehensive care outside traditional hospital settings. This evolution underscores a huge shift towards integrating advanced technology to enhance patient outcomes and at-home healthcare.
Here’s why:
- Early Intervention: By continuously tracking vital signs, healthcare providers can quickly and easily detect early signs of deterioration or complications, enabling timely interventions, preventing adverse events.
- Better Outcomes & Lower Costs: This proactive approach not only improves patient outcomes but also reduces the need for hospital readmissions and associated healthcare costs.
As a result, proactive monitoring proves to provide patient, physician and healthcare system benefits that are shaping the future of Hospital-at-Home programs.
Study Demonstrates Benefits and Effectiveness of Hospital-at-Home Programs
A reputed Hospital-at-Home study: Hospital at home: emergence of a high-value model of care delivery – PMC demonstrated that Hospital at Home provides numerous benefits, especially for the elderly and those with chronic conditions. It reduces costs by minimizing hospital stays and diagnostic tests while lowering readmission rates and improving clinical outcomes. It also decreases the risk of hospital-acquired infections and enhances patient comfort and satisfaction. Hospital-at-Home also supports high-demand situations with a flexible, scalable model that integrates technology, processes, and supply chains, ultimately easing the strain on traditional hospitals and offering a viable alternative for acute care.
Biometrics – The Key to Success
A concern for clinicians is the challenge of effectively processing and responding to the influx of data coming in from Hospital-at-Home programs. To understand the level of effort required to virtually monitor hospital-at-home patients and to assess the frequency of escalations, clinical researchers at Best Buy Health conducted an analysis with UMass Memorial Health (tracking over 300 patients) focused on the staff time required to manage the data and alarms generated by continuous monitoring of high acuity patients.
The findings shed light on the game-changing impact of continuous monitoring on patient care:
- Escalations to hospital staff were rare, happening just once per 132 monitored patient hours.
- Most alarms didn’t require direct patient contact thanks to prior communication or built in redundancy.
- Virtual nursing also stepped up to the plate, clocking over 64 hours of engagement to further relieve the burden to providers.
Training, Knowledge & Skills
The transition for clinicians from traditional hospital settings to monitoring biometric data in alternative contexts represents a significant paradigm shift. The unfamiliarity of the environment and the nuanced nature of the data can evoke feelings of uncertainty among professionals.
This shift emphasizes the pressing need for in-depth training programs tailored to equip healthcare professionals with the knowledge and skills necessary to navigate the complexities of continuous monitoring effectively. Moreover, it emphasizes the importance of recalibrating approaches to alarm management, recognizing that the thresholds for alarm in these settings may differ substantially from those in traditional hospital environments.
By integrating recommended alarm thresholds and re-evaluating their approach to alarming, clinicians can enhance patient care and safety in remote monitoring scenarios. Ultimately, adopting a proactive mindset towards continuous monitoring, coupled with comprehensive training and monitoring protocols, is essential in ensuring optimal patient outcomes in evolving healthcare landscapes.
CONCLUSION
In summary, the growing adoption of Hospital-at-Home systems and collaborations like these enrich the recovery of patients by providing high-quality, personalized care in the comfort of their homes.
Hospital-at-Home programs, supported by advanced Remote Patient/Physiologic Monitoring (RPM) tools, are proven to be safer, more cost-effective, and more efficient than traditional hospital care, particularly for vulnerable patients at risk of hospital-acquired infections.
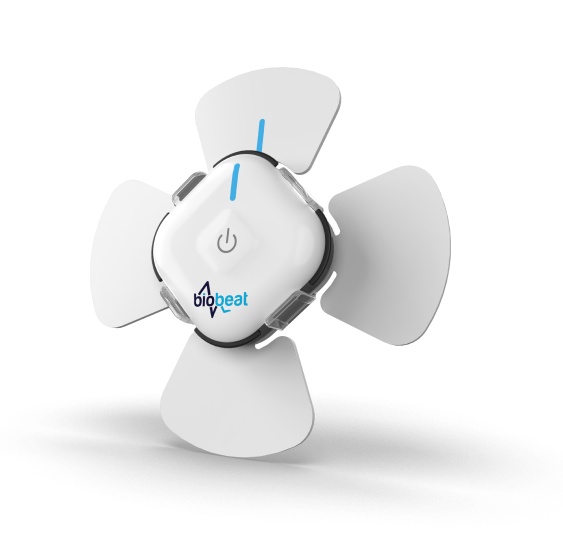
Continuous monitoring devices, such as those developed by Biobeat, offer comprehensive solutions with 13 medical vital signs, FDA and CE approvals, and advanced health-AI platforms that enhance patient outcomes through real-time early warning scores and data-driven decision support. These innovations ensure that Hospital-at-Home programs can deliver the same level of care as hospitals, reducing complications, lowering costs, and improving overall patient satisfaction.